Biotin 10000µg 120 Tablets
Mag 24-7 Magnesium Citrate 500mg 120 Capsules
NAC N-Acetyl-Cysteine 600mg 120 Vegetarian Capsules - 4-Month Supply
Cherry Go Montmorency Cherries 1500mg 90 Capsules
K2D3 Fusion Vitamin D3 3000 IU and Vit K2 100ug MK7 90 Capsules
Organic Turmeric 500mg with Black Pepper Extract 120 Capsules
Vitamin B12 Methylcobalamin 1mg 120 Capsules
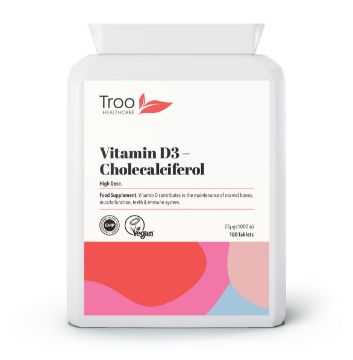
Vitamin D3 25mcg 1000iu 180 Vegan Tablets
Vitamin D3 4000iu 365 Tablets - 1 Year Supply
FloraFusion Advanced Probiotics 60 Capsules - 30 Strain 22.5 Billion CFU
FloraFusion Elite Advanced Probiotic 60 Capsules - 30 Strain 45 Billion CFU
Radiance HSN Hair Skin & Nails Complex - 150 Raspberry Flavour Gummies
FocusFusion Plus Brain Support 60 Capsules - Focus & Concentration
Vitamin D3 4000iu - 150 Orange Flavour Gummies - High Strength
Ashwagandha 600mg - 150 Natural Raspberry Flavour Gummies
Vegan Omega 3 Algal Oil 90 Softgels - High Strength EPA & DHA
Folic Acid 400μg - 120 Natural Berry Flavour Gummies
Apple Cider Vinegar Ginger - 120 Natural Apple Flavour Gummies
Organic Lions Mane Extract with Acerola Black Pepper 120 Capsules
Probio Cult-20 Complete 20 Billion CFU 120 Capsules
Rosehip Extract 5000mg Vitamin C 120 Capsules
Saw Palmetto 2500mg from 125mg 20:1 Extract 90 Capsules
Welcome to Troo Health
Welcome to Troo Health
Founded in 2009, Troo Health has built a long and trusted reputation for providing high quality supplements that you and your family can rely on. When you put your faith in Troo Health you can do so with complete peace of mind - your satisfaction is our priority!
All Troo Health supplements are manufactured in the UK to GMP standard to ensure consistently high quality and safety. Troo Health has attained and works to ISO 9001:2015 quality management certification, continually working to ensure the systems we use are best placed to serve your needs. We are also an earth positive business, working in conjunction with Greenspark to ensure we meet our environmental responsibilities, including a commitment to plant a tree for every order placed on our website.
Whether nutritional support for you or your pets, you can rely on Troo Health do be there for you. Our team of nutritional experts are on hand to address any concerns or queries you may have, so please feel free to ask us a question.
Welcome to the Troo Health family.